
S.T.EYE condom: A revolutionary approach to STI detection
Image: Anna Shvets
Imagine a world where a simple colour change could alert you to a sexually transmitted infection (STI), protecting your health and that of your partner.
That’s the groundbreaking vision behind the S.T.EYE condom, a conceptual innovation by three British teenagers. Still in the idea stage, this invention could address a major public health challenge: rising antibiotic-resistant STIs.
Let’s dive into how this concept works, its potential impact, and why this innovation could be a game-changer for global sexual health.
The S.T.EYE condom is no ordinary contraceptive. It is the brainchild of Daanyaal Ali and Chirag Shah, both 14, and 13-year-old Muaz Nawaz. Its unique feature is a colour-coded system that can detect STIs.
Using antibodies embedded in the condom, it reacts to STI-specific proteins (antigens) present in bodily fluids.
Just as a home pregnancy test uses antibodies to detect specific hormones and change colour in response, the S.T.EYE condom functions similarly. When chlamydia antibodies within the latex come into contact with antigens, they bind together, triggering a colour shift that indicates the presence of the infection.
When an STI is detected, the condom would change colour: green for chlamydia, blue for syphilis, yellow for herpes, and purple for HPV.
This idea was inspired by ELISA testing, a diagnostic method that uses colour changes to detect diseases.
Ali explained, “Once bodily fluids contact the latex, if the person has any STI, the antibodies in the condom react and cause a visible colour change.”
What makes this innovation particularly intriguing is its potential to offer private, immediate, and stigma-free STI detection. No awkward clinic visits or long waits for lab results, just instant information in the privacy of your home.
Sexually transmitted infections are not just a personal health issue; they’re a public health crisis.
If there’s anywhere in the world that would benefit from an STI-detecting condom, it’s South Africa.
According to South Africa’s National Institute for Communicable Diseases (NICD) and recent surveillance studies (2021–2024):
And the numbers don’t lie. With 8 million people living with HIV, untreated STIs increase both transmission risk and long-term complications.
The most common and serious complications of untreated STIs include pelvic inflammatory disease (PID), infertility, certain cancers, and severe pregnancy and birth complications. Untreated STIs also increase the risk of contracting or transmitting HIV.
The journey to creating the S.T.EYE began in a classroom in Ilford, London, during a TeenTech competition that challenges students to use technology to solve real-world problems.
The boys stumbled upon a Reddit post that suggested a colour-changing condom and decided to make it a reality by adding the STI-detection twist.
“We wanted to make life simpler, easier, and better,” said Nawaz.
Their teacher introduced them to the concept of antibodies and antigens, which became the foundation for their design. What started as a school project quickly gained international attention, earning them the TeenTech award and a meeting with the Duke of York at Buckingham Palace.
Their innovation has already garnered interest from condom manufacturers, sparking hope that this concept could one day reach the market.
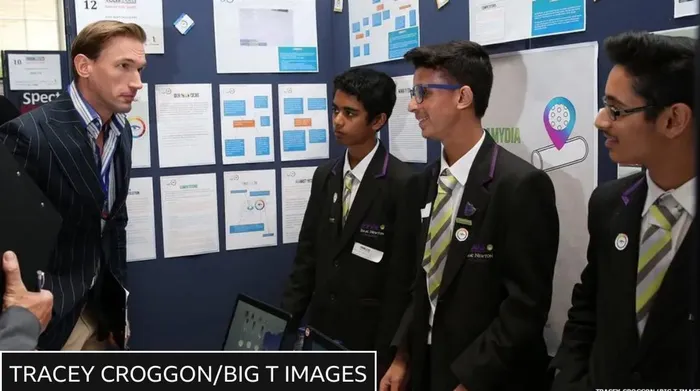
Muaz, Daanyaal and Chirag talk to Dr Christian Jessen from Embarrassing Bodies, one of the TeenTech judges
Image: BBC
But can it actually work?
Sexual health expert Dr Mark Lawton, consultant in sexual health and HIV with the British Association for Sexual Health and HIV (BASHH), says the science is promising but complex
While the idea is undoubtedly promising, turning it into a commercially viable product is no small feat. Scientists and experts in the field have pointed out several hurdles:
1. Technological feasibility: Can the antibodies embedded in the condom reliably detect multiple STIs without cross-reactions or inaccuracies?
2. Safety concerns: Would the chemicals used for detection be safe for human contact over prolonged periods?
3. Behavioural impact: According to the BBC, Dr Mark Lawton, a consultant in sexual health and HIV, posed a question, “Would people avoid using condoms if they feared being ‘found out’ or judged by their partner?”
Despite these challenges, Lawton praised the teenagers’ creativity and their commitment to addressing a real-world issue. “This technology could be possible, but additional research and testing are needed,” he noted.
As antibiotic resistance grows and STIs continue to spread, the need for innovative solutions has never been more urgent. The S.T.EYE condom may still be a concept, but it represents a bold step toward a future where sexual health is safer, simpler, and more accessible for all.