How South Africa's ICU bed crisis threatens lives in the public health system
As South Africa grapples with a critical lack of ICU beds, countless lives hang in the balance.
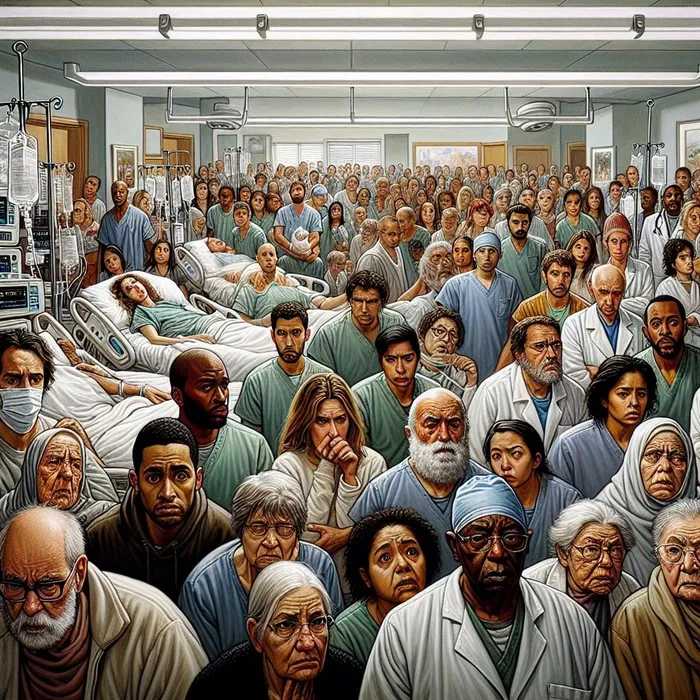
Image: IOL / Ron AI
A critical shortage of Intensive Care Unit (ICU) beds in South Africa's public healthcare system is producing tragic consequences, with citizens facing death and deteriorating health as a result.
This alarming situation has been underscored by research from Professor Fathima Paruk, revealing that the nation has a mere five ICU beds per 100,000 people — a stark contrast to Germany's 39. In some provinces, the situation is even dire, with reports indicating as few as one ICU bed available.
The implications of this bed scarcity are deeply personal for many, including Yolanda Dyantyi, who is mourning the loss of a close friend from Gauteng.
Dyantyi alleges that her friend’s death was exacerbated by the critical shortage of ICU beds, a plight she attributes in part to what she terms “corruption led by the political elite”.
Her friend suffered multiple seizures and, in a harrowing series of events on September 4, 2025, was rushed to a hospital.
Dyantyi maintains that it took an agonising hour to secure medical attention due to “service delivery issues” within both the public and private healthcare systems.
Eventually, she said, due to a lack of ICU beds, he was admitted to a private hospital before being transferred to a well-known public facility after several days, as he could not afford medical aid. He fought for his life in the ICU until he succumbed to his condition on October 1, 2025.
“The violence of it all is what is heart-wrenching for me,” Dyantyi reflected. “He was just 29 and his body turned against him. It feels so inexplicable.”
Her friend's tragic experience has resonated widely. In response to Dyantyi's tweet on X, another woman shared her family's struggle: “My dad waited six weeks for an ICU bed for a bypass. Before it happened, the gangrene spread and he is now a double amputee.”
A Durban doctor, who chose to remain anonymous, echoed the sentiment that the public healthcare system is in crisis, particularly regarding ICUs.
The GP's observations paint a troubling picture of a sector struggling with severe funding limitations and widespread corruption, significantly diminishing its ability to care for critically ill patients.
A major contributing factor is the critical shortage of dedicated ICU specialists, primarily due to insufficient state salaries, he said.
Patients with life-threatening conditions like cardiac or renal failure are often relegated to general wards, lacking necessary specialised care.
“Poorer patients often face a lack of available beds, leading to treatment in passageways,” the doctor noted.
He stressed this is alarming for severe conditions like heart attacks; many are discharged without optimal medical attention.
“Doctors will tell you, we’ll give you medicine, and sometimes people die in the ward or at home. People go at 3am and are only seen at 4pm; sometimes they wait all day or are told to return another day.”
In KwaZulu-Natal, patients needing cardiac ICU care at facilities like Addington or Mahatma Gandhi hospitals are often transferred to Inkosi Albert Luthuli Hospital — if a bed is available.
According to the doctor, these issues have persisted for years, especially post-Covid-19. In contrast, the private healthcare sector appears to thrive.
“Every day in the ICU, the doctor can just say ‘hi’ and get R3,000. In the general ward, they only get R800,” he stated.
While it seems the private sector meets demand, it too is straining. The doctor noted that private ICUs are overcrowded as specialists admit patients who could receive adequate treatment in general wards into ICUs instead.
“After patients get better, they keep them there for the whole week. Then doctors have to call different hospitals to check for available beds.”
Dr Nonkululeko Boikhutso, CEO of Nelson Mandela Children's Hospital, affirmed the severe shortage of ICU beds in the public sector, attributing it to an overwhelming volume of patients.
Boikhutso explained that doctors and hospital managers often have to call other institutions to find available ICU beds.
“We sit with bed utilisation rates above 95% for ICU beds. A 2022 study from KZN showed there were 0.73 beds per 100,000 children compared to a need of 23.7 per 100,000 children,” she said.
The greatest impact is on patients awaiting elective surgeries who may need post-operative ICU beds.
“This means they have to wait weeks or months to access these services. In our hospital, children cannot get heart operations, or they face delays due to the unavailability of ICU beds,” said Boikhutso.
This problem is not unique to her hospital, she said. There is a chronic shortage of medical specialists in South Africa, particularly in critical care.
“The general physician-to-population ratio for South Africa is 0.809 per 1,000 people, compared to 3.7 per 1,000 in more developed countries,” she stated.
The nursing shortage is even more acute, as one nurse is needed per patient in the ICU, she emphasised.
Boikhutso referenced an article by M Matlakala published in 2023, stating that there are 6,246 registered nurses in South Africa with critical care specialisation.
“This is about 0.1 nurses per 1,000 population, far below the 6-8 per 1,000 seen in developed countries,” she said.
Critical care is a rare skill for both nurses and doctors. Although training for critical care doctors continues in South Africa, nursing numbers are shrinking as post-basic training for critical care and other subspecialties is not occurring.
A Gauteng study found that 59.1% of ICU nurses have critical care qualifications.
“We also face a brain drain from the public sector to private and to the Middle East, where competitive packages are offered,” added Boikhutso.
Boikhutso advocates for reviewing nursing training regulations and increasing healthcare investment, particularly where population growth strains services.
She noted that South Africa produces doctors who cannot be absorbed or trained as specialists, leading many to private practice or emigration.
Echoing this view, Dr Imran Keeka, DA spokesperson on Health, agreed that there is a definite shortage of ICU beds across the province, though he does not have a breakdown of the exact number per hospital.
“With the rising burden of disease and trauma, the demand far exceeds the available capacity,” he said, adding that there is also a critical shortage of specialised nurses and ICU doctors.
Keeka said expanding the number of beds is not simply about infrastructure; it requires trained staff, resources, and in the current fiscal climate, this is extremely difficult.
For example, Grey’s Hospital alone has identified a need for at least 10 additional ICU beds, and while they believe they can just about manage the staffing, it would stretch existing capacity.
He explained that regional and district hospitals, like Northdale, are often forced to provide services they are not equipped for due to shortages, causing delays for vulnerable patients needing urgent intensive care.
Keeka said the shortages stem from a combination of increased patient load, limited training pipeline for critical care personnel, and funding constraints.
Addressing this issue will require a phased expansion of ICU capacity, investment in staff training, and a stronger focus on the retention of skilled professionals, he noted.
“Overall, ICU bed shortages are present at all levels of care and across all disciplines - from paediatrics to cardiology,” said Keeka.
The Health Department did not respond to requests for comment but reported last month that it could not confirm the exact number of national ICU beds due to a lack of recent audits. Future interventions will be based on Prof Paruk's findings.
Foster Mohale, department spokesperson, noted that ICU planning considers both public and private capacity.
However, he emphasised that ICU care also requires highly trained specialists, and patients are often stabilised in smaller hospitals before transfer to ICU-equipped facilities.
The Critical Care Society of Southern Africa said Professor Paruk had quoted the findings of National Audit publications, which were last conducted several years ago.
The CCSSA agrees with Paruk that a repeat audit is urgently needed due to changes in critical care, largely influenced by the Covid-19 epidemic.
“As such, the CCSSA will be conducting the national audit in 2026 to get a clearer picture of the status quo.”
Have thoughts on this topic or other subjects you’d like us to explore? Want to share your experiences? Reach out to me at karen.singh@inl.co.za – I’d love to hear from you!