Study cautions against reducing South Africa's medical internship programme.
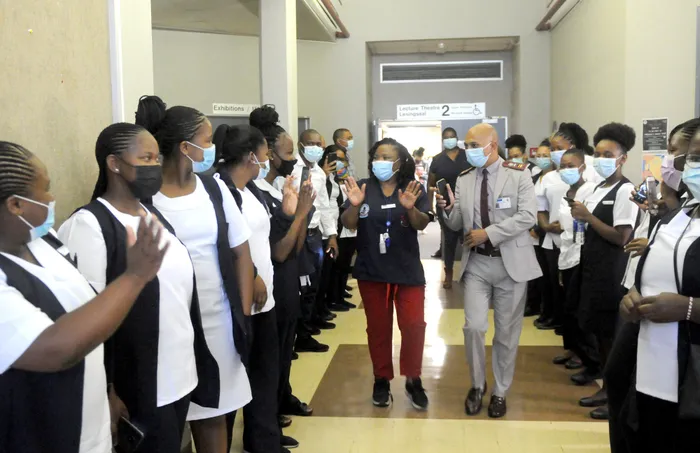
Image: Ayanda Ndamane/African News Agency(ANA)
A recent study conducted by the University of Cape Town (UCT) has brought to light ongoing challenges within South Africa’s two-year medical internship programme, especially in surgical training. The research sheds a critical spotlight on proposed initiatives to shorten the internship period, cautioning that such moves could jeopardise the clinical exposure and preparedness of junior doctors entering the healthcare system.
Published in the esteemed BMC Medical Education journal, the survey sufficiently canvassed the sentiments of 82 participants—comprising 63 medical interns and 19 experienced clinicians, such as intern curators and heads of department—based in the Western Cape. According to the findings, most interns regard the two-year structure of the internship as a vital transition from academic training to independent medical practice.
Overwhelmingly, more than two-thirds (68%) of those surveyed believed that reducing the internship duration to a single year would be detrimental, with respondents warning of significant repercussions, including diminished clinical exposure (83%) and reduced teaching time (75%). “The data clearly indicate that interns and supervisors believe the two-year internship remains vital for developing competent, confident doctors ready to serve South Africa’s health system,” said Professor Salome Maswime, co-author of the study and head of UCT’s Global Surgery Division.
Interns expressed satisfaction with their readiness for independent work across various specialties, citing impressive preparation in family medicine (96%), anaesthesia (94%), psychiatry and mental health (86%), internal medicine (81%), paediatrics (76%), and obstetrics and gynaecology (71%). Nevertheless, only 38% felt adequately prepared by their surgical rotation, highlighting issues related to limited procedural opportunities and guidance within surgical departments.
When asked about their aspirations during the internship, interns outlined a desire for hands-on experience and mentorship. A substantial 90% wanted to enhance their procedural skills, while 89% aimed to refine their diagnostic capabilities, and 84% highlighted the importance of substantial interaction with senior colleagues to bolster their learning.
Professor Maswime emphasised that the findings reinforce a critical need for the internship to maintain its focus on clinical immersion and practical skill development. This is particularly essential in high-pressure environments that reflect the realities of medical practice. “Direct experience within a discipline is key to improving confidence and preparedness, a principle that resonates across all levels of care,” she explained.
With a growing population and a notable decline in available medical specialists per capita, the demand on junior doctors for patient care continues to escalate. This challenge is further intensified by the increasing prevalence of medically complex patients, a trend influenced by greater life expectancy due to widespread antiretroviral therapy, according to Maswime.
The survey underscores the importance of robust exposure to foundational medical fields such as family medicine during internships, which is crucial for equipping junior doctors for diverse healthcare settings. Additionally, Maswime pointed out that reasons leading interns to shy away from rural and primary care must be systematically identified and mitigated to enhance service delivery to the larger population.
“Efforts to create a family medicine rotation that is fit for purpose should continue to be promoted, offering opportunities that connect aspects of rural healthcare with junior doctors’ future practices, thereby encouraging them to remain in these crucial roles,” she concluded.
Related Topics: